From abortion to Hurricane Helene to medical debt, here’s what drew readers to NC Health News in 2024

By Rose Hoban, Will Atwater, Jaymie Baxley, Anne Blythe, Michelle Crouch, Rachel Crumpler, Taylor Knopf and Grace Vitaglione
When the NC Health News team took a stab at the start of the year at predicting what health-related issues would guide our coverage throughout 2024, there was no question that politics and the campaigns for president, governor and other state offices would play a large role.
And they did.
But we had no idea about the devastation that Hurricane Helene would bring to western North Carolina and all the news the catastrophic storm would generate the last quarter of this year.
As we look back on the year that was, some of the most-read NC Health News stories included articles about Helene’s effects, from its upheaval of municipal water systems to the use of cadaver dogs and other issues that arose during the aftermath of the havoc generated by the storm.
Readers also were drawn to coverage about health care costs, Medicare Advantage and medical debt. There was great interest in the investigations into state-supported behavioral health management agencies and a psychiatric hospital in eastern North Carolina.
Two issues that drew reader interest in 2023 — abortion access and pandemic-related rules — also brought readers to the site in 2024.
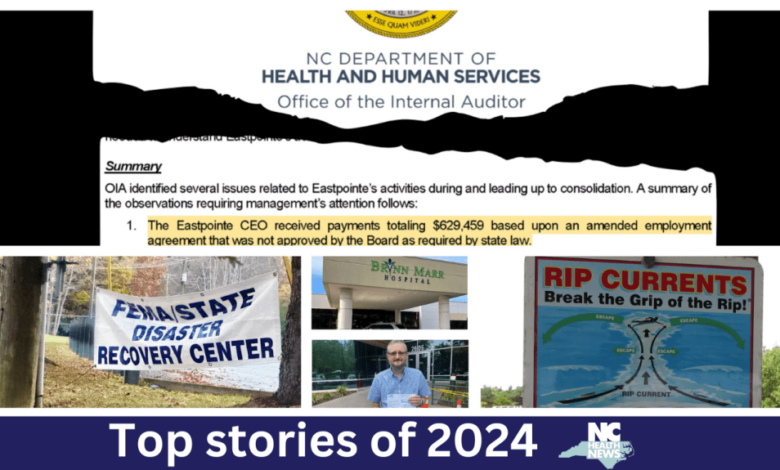
Rip currents are active year round
Our most-read story last year had to do with a quintessentially North Carolina concern: beach safety. We wrote about the powerful rip currents that pop up along the coast, particularly when there’s an offshore storm. Last summer, rip currents were a prominent fixture along the North Carolina coast, with more than 600 people rescued from southeastern North Carolina beaches in Brunswick, New Hanover and Pender counties during 2024’s summer season, according to National Weather Service Meteorologist Tim Armstrong.
The National Oceanic and Atmospheric Association defines rip currents as powerful, narrow channels of fast-moving water on shorelines. They tend to form where waters with less wave-breaking action are “sandwiched between water with greater wave breaking.”
NOAA notes that rip currents “are found on almost any beach with breaking waves and act as ‘rivers of the sea,’ moving sand, marine organisms, and other material offshore.”
Last summer’s rip current activity was linked to an above-average hurricane season, according to meteorologists. Hurricanes can be hundreds of miles or more away from shore and still trigger rip currents.
Rip currents are also active in the colder months and are linked to winter coastal storms or nor’easters.
“It’s not like they go away in the winter,” said Erik Heden, warning coordination meteorologist for the National Weather Service in Morehead City. “It’s just that nobody’s swimming in 40- to 50-degree water. If they are, they’re in a bodysuit and are surfers, [who] know what they’re doing.”
Wyatt Werneth, public service spokesperson for the American Lifeguard Association, agrees.
“Believe it or not, winter swells actually cause more rip current activity than the summer swells, minus the hurricanes,” Werneth said. “You know, hurricanes obviously brew up your strongest conditions, but the way winter swells come in, they are usually a little bit more aggressive.”
Werneth added: “We’re fortunate that more people seem to stay out of water when it’s cold, but the rip currents are always a threat, and people should always think about that.”
Heden said the peak rip current season is April to October. This coincides with the Atlantic Hurricane season, which encompasses the season when people are more likely to be in the water.
— Will Atwater
DHHS audit of mental health agency finds millions in payments to executives, law firm ahead of merger. Now their board will be reconfigured.
As of Dec. 30, Trillium Health Resources, the mental health management agency providing services to 46 mostly eastern North Carolina counties, has a new board of directors.
The move was initiated by North Carolina Health and Human Services Secretary Kody Kinsley in response to ongoing turmoil on the board of the agency, which is on the receiving end of billions in state and federal dollars.

Near the end of 2023, Kinsley was empowered by the General Assembly to force a consolidation of Eastpointe Health Services, which had served 10 counties, the Sandhills Center, which served 11 counties, and Trillium. The consolidation resulted in a slimmed-down board that kept some board members from all three agencies.
Months after the forced merger, a scathing DHHS audit revealed that as Eastpointe was preparing to sunset, former CEO Sarah Stroud and former Chief Business Officer Catherine Dalton were given more than a million dollars combined in severance, benefits and bonus packages. The late-December payments to Stroud and Dalton were approved by the Eastpointe board chair, Greene County Commissioner Jerry Jones, but according to the audit, neither payment was approved by the full board — something required by state law.
In the closing hours of Eastpointe’s existence, the two women also deleted thousands of emails, something that’s illegal under North Carolina state law.
During the same time period, Eastpointe’s legal counsel was paid more than $3 million in charges backdated to 2021.
Jones, who approved the payments to Stroud, Dalton and the general counsel (the Charleston Group), remained on the new Trillium board. Minutes of the combined board meetings from early 2024 reviewed by NC Health News show ongoing tension between board members. That tension was on display during a nearly four-hour meeting in March where members from the old Eastpointe board launched an unsuccessful attempt to force through new governing bylaws that would have diminished the role of mental health consumers and family members, something that goes against state law. The revised bylaws would have given power to board members from the now-shuttered organizations.
Kinsley made substantial structural changes in the new board which he mandated creation of as of Monday. The new board — which only retains five members from the 2024 board — will have one-third members who are consumer advocates, and diminishes the role of county commissioners, who had been nearly half of the old board.
“I find that it will allow for culturally diverse feedback from the local communities, allow for continued county involvement, and provide for equitable representation across the catchment area as well as relevant expertise,” Kinsley wrote in his directive.
NC Health News broke the news of the audit, in a story that was our second-most read of 2024. To date, no funds have been returned — nor have there been charges filed.
— Rose Hoban
In wake of deadly Helene, western N.C. thirsts for water
The western part of the state had already received a torrent of rain over a four-day period in late September when the remnants of Hurricane Helene tore through the mountainous region’s craggy landscapes, rippling creeks and meandering rivers.
The deluge of water dropped by the storm caused extensive flooding and devastation, 103 verified storm-related deaths and billions of dollars in damages that are likely to trouble the region for years to come.
Paradoxically, so much water everywhere created a water shortage for months in parts of the storm-ravaged area. Power outages, the destruction of much of Asheville’s municipal water system and more left survivors on an immediate hunt for drinkable water.
As of Sept. 29, as NC Health News reported, 145 water systems were either without power, suffering infrastructure damage or under boil-water alerts, which meant individuals, businesses and health care systems were without a fundamental resource.

“There is a massive effort going on now to move water and other supplies into these affected areas because we know that they’re going to be needed,” Gov. Roy Cooper told NC Health News during a Sept. 29 storm update.
State Sen. Ralph Hise, a Spruce Pine Republican, lamented the loss of the Mitchell County water treatment system.
“The tanks don’t hold water anymore,” he said. “All of the electronics are gone, two of the buildings are gone that were at the center.”
There were no quick fixes for the Asheville water system. For weeks, city officials refused to release a timeline for when people might have safe drinking water flowing into their households and businesses.
Even safe, nonpotable gray water, which could be used for flushing toilets and other household needs, was difficult to come by for a while.
Buncombe County officials urged residents to stay away from the rivers for such purposes, saying the French Broad, the Swannanoa and others “should be treated as basically a hazmat site.”
“Please do not touch the water or get near the water if you do not have to,” Stacey Wood, a Buncombe County spokesperson, said during an Oct. 4 storm update. “There are other resources. We will make other resources available to you if that is your circumstance.”
By mid- to late October, Asheville had restored heavily chlorinated — but still non-drinkable — water to 95 percent of the system users.
But murky reservoirs and elevated lead levels further complicated a return to more of a sense of normalcy. Now, lead test kits are being distributed by the city.
A greater demand for wells also rose in the storm aftermath.
The recovery and rebuilding will continue into 2025 and beyond.
— Anne Blythe
When your MD visit comes with a hospital fee, but no hospital
Frustration with medical billing reached new heights in 2024 as patients continued to grapple with rising health care costs and opaque billing practices. Among the most egregious charges: surprise hospital facility fees for routine doctor visits.
Traditionally, facility fees were added to hospital bills to help cover the higher overhead costs of operating a 24/7 hospital. However, as health care systems snapped up medical practices and clinics, they started tacking the fees on to bills for patient visits miles away from a hospital campus.
In one case highlighted in a September article, a cancer patient was charged hundreds of dollars more after Novant Health acquired her oncology practice, even though she had been seeing the same doctor in the same building at a lower cost before the acquisition.
At least 15 states have taken action to address facility fees, according to the National Academy for State Health Policy. At the federal level, Congress considered — but did not implement — so-called site-neutral payments, which would require Medicare pay hospital outpatient clinics the same amount for the same service as at an independent physician’s office.
In North Carolina, Sen. Jim Burgin (R-Angier) co-sponsored legislation in 2023 and 2024 to limit facility fees. The North Carolina Healthcare Association, which represents the state’s hospital community, opposed the measure, arguing that the fees are crucial to cover the higher costs associated with hospital-level care.
Burgin said he plans to try again in 2025.
– Michelle Crouch
‘Something from a horror novel’: U.S. Senate slams owner of N.C. psych hospitals
In May, NC Health News and WRAL-TV co-published a two-part investigation into Brynn Marr Hospital in Jacksonville in which more than a dozen former employees alleged the psychiatric facility was a chaotic, violent place for staff and patients. Former staff members of the for-profit hospital claimed that understaffing and frequent turnover led to unchecked violence from patients and conditions that allowed patient-to-patient sexual assault.
Former employees told NC Health News that they were instructed by hospital management to falsify records — including documenting more severe diagnoses for patients to make them appear sicker than they were — so that Brynn Marr could send higher bills to insurers. The former staff members also alleged that hospital officials pushed medication over therapy while offering little in the way of mental health treatment.
Brynn Marr’s chief executive at the time denied the allegations made by the former employees.
A month later, a U.S. Senate committee released a blistering report titled “Warehouses of Neglect” that accused four of the nation’s largest for-profit behavioral health companies — including Brynn Marr’s parent company Universal Health Services — of putting profits above the safety and treatment of children placed in their care. Universal Health Services manages nearly a quarter of North Carolina’s licensed inpatient psychiatric beds.
The Senate report was the result of a two-year investigation by the office of Senate Finance Committee Chair Ron Wyden (D-Oregon), which found that these facilities often provide minimal therapeutic treatment in poor physical settings with inadequate staffing, maximizing profits at the expense of patient care. The report documented numerous instances of harm to children in these facilities, including self-harm, patient escapes, child fatalities, sexual abuse and improper use of seclusion and chemical restraints.
Universal Health Services said in a statement: “We vehemently dispute this characterization of our facilities.”
The Senate committee’s report calls for raising standards of care and increasing oversight of residential psychiatric facilities. Lawmakers in North Carolina, nonetheless, have proposed budgets that keep funding flat for the state’s regulatory agency responsible for oversight.
Mental health advocates argue that instead of relying on these problematic residential facilities, the focus should be on expanding community-based mental health services to help people before their symptoms escalate into a crisis. They say this would reduce the need for residential treatment and the associated risks of abuse and neglect.
In June, Wyden said he would introduce federal legislation to raise health and safety standards, require oversight and enforcement, and invest in community-based mental health services. As leadership in the U.S. Senate shifts to Republicans, the senator said he still plans to release legislation to address these systemic mental health problems early next year, according to Nicole L’Esperance, a spokesperson for Wyden.
“Even without the gavel next year, Wyden will continue to work on these issues. He’s not letting up,” L’Esperance wrote in an email in November. “Right now, getting that legislation is top priority.”
— Taylor Knopf
How dogs search for the lives taken by Helene in western N.C.
The flooding rains and gale-force winds generated by the remnants of Hurricane Helene claimed at least 103 lives in western North Carolina, making it one of the deadliest natural disasters in the state’s modern history.
The human toll of September’s catastrophe was not immediately apparent, because it took time to find the bodies of storm victims in the region.
Search teams used highly trained dogs to find the remains of dozens of people who had been buried beneath rubble and floodwater. These specialist canines and their handlers helped give closure to victims’ families in the days and weeks after the storm.

Cat Warren, a North Carolina-based cadaver dog trainer who wrote a 2013 bestseller about the science and history of working dogs, spoke to NC Health News about the grim but essential service provided by canine-assisted crews in Helene’s wake.
“It takes absolute experience for the dogs and handlers to work in these situations,” she explained in an interview published on Nov. 4. “Very often, they are working through mud, or they’re on a boat going down very swollen rivers or lakes. They have to be physically fit and enormously resilient.”
Thankfully, nearly all of the missing residents in the affected counties have been located as of early December, with only a handful of people who remain unaccounted for.
— Jaymie Baxley
Medicare Advantage popular but troubled
Older North Carolinians joined Medicare Advantage plans in higher numbers this year, even as the program faces increasing scrutiny.
Over half of the 2.2 million Medicare-eligible North Carolinians are in Advantage plans. Instead of “traditional” Medicare, where the federal government pays for every beneficiary’s test, appointment or hospital stay on a fee-for-service basis, in Medicare Advantage, the government pays private insurance companies to administer care for a set per member monthly amount.
Some older adults told NC Health News they like the extra benefits associated with Medicare Advantage plans, such as hearing and dental coverage, or even gym benefits.
But others said they’re nervous about the possibility of their doctors leaving the more limited networks created by the plans.
Meanwhile, some companies that offer Advantage plans are facing pushback from federal regulators for forcing doctors and patients to jump through hoops before approving care — a process known as prior authorization — and allegedly gaming the system to receive higher government payments.
Throughout this year, the Biden administration took tentative steps to curb overpayments from the government to Medicare Advantage, as well as address the inappropriate use of prior authorization hindering access to care.
The future of the Medicare Advantage landscape is uncertain. President-elect Donald Trump’s nominee to lead the Centers for Medicare and Medicaid Services, Mehmet Oz, has been a supporter of Medicare Advantage, Politico reported.
Medicare Advantage beneficiaries may switch to a different Advantage plan during the upcoming Medicare Advantage open enrollment period, which runs from Jan. 1 to March 31.
— Grace Vitaglione
Abortion limits at one year
July 1, 2024, marked one year into North Carolina’s stricter new abortion law — Senate Bill 20 — which passed despite the objections of medical professionals and over Gov. Roy Cooper’s veto. The law reduced the time frame for seeking most abortions from 20 weeks of pregnancy to 12 weeks and added an in-person requirement for state-mandated counseling at least 72 hours before an abortion.
Abortion providers told NC Health News they faced their toughest year yet adjusting to a new landscape of care. Clinic staff reworked operations to comply with the law and adapt patient flow. They’ve also increasingly had to expand their role beyond providing medical care, doing more coordination to help patients navigate to other states to receive care past the 12-week North Carolina limit.
For patients receiving an abortion in North Carolina, the state’s abortion law requires them to visit clinics at least twice — and many need to travel long distances to those clinics. The state has 14 abortion clinics, which are concentrated in nine counties. The additional appointment means extra time off work and more travel,hotel stays and child care costs for patients, which adds logistical hurdles to care.
Despite the new restrictions, abortion volume in North Carolina has not dropped significantly since Senate Bill 20 took effect, according to data from the Guttmacher Institute, a national organization that tracks trends in reproductive health. In large part, that’s due to the efforts of abortion clinics, providers, abortion funds and other support networks that have worked to keep abortion accessible.

The more restrictive law has also complicated abortion training for the next generation of OB-GYNs, who now have limited exposure to second-trimester abortions, which can be more technically challenging. In response, medical schools in North Carolina have made adjustments, including more simulation work and arranging training opportunities out of state for hands-on experience in a less restrictive environment.
— Rachel Crumpler
Doctors rail against proposed ban against public masking
North Carolina lawmakers got an earful when they proposed rolling back a pandemic-era law that permitted people to wear face masks for public health purposes.
The measure was part of a bill that also reformed campaign finance laws for federal-level political action committees and political party committees, creating pushback from Democrats questioning the relationship between the two topics.
Health care providers and others criticized the Republican-led General Assembly for trying to do away with a public health exemption adopted in 2020 that changed an anti-masking law that has existed since 1953. The statute was adopted 71 years ago, in part, to prevent Ku Klux Klan members from wearing masks, hoods and other devices to conceal their identities and voices in public spaces.
The proposed rollback came as many college campuses were seeing large gatherings of people protesting the Israel-Gaza conflict. Many in attendance wore face masks and sunglasses that made it difficult for law enforcement agencies to use facial recognition tools to identify people exercising their free speech rights.
Face masks became one of the tools used throughout the pandemic to reduce the spread of COVID-19. Since then, many people use them to try to protect themselves from respiratory viruses, to reduce allergic reactions and to prevent the spread of illness to others.
The possibility that they would be banned in North Carolina, save for a few extenuating circumstances, drew widespread rebuke. Even Jerome Adams, a surgeon general during the first Trump administration, weighed in with concerns on social media. “It’s disturbing to think immunocompromised and cancer patients could be deemed criminals for following medical advice aimed at safeguarding their health,” said Adams, whose wife has been treated twice for melanoma.
Opposition from several Republicans forced an amendment of the initial proposal.
Ultimately, the legislation (HB237), which survived a veto by Gov. Roy Cooper, allows the wearing of “a medical or surgical grade mask for the purpose of preventing the spread of contagious disease.”
— Anne Blythe
New state program targets medical debt
In July, North Carolina launched an ambitious medical debt relief program designed to reduce the burden of medical debt on low- and middle-income patients.
The program, the first of its kind in the nation, offers additional federal payments to hospitals that agree to forgive old medical debt and beef up their charity care policies.

All 99 of the state’s acute care hospitals agreed to participate, committing to forgive approximately $4 billion in medical debt for nearly 2 million patients. In return, the hospitals will receive millions of dollars in boosted federal payments associated with the state’s expansion of Medicaid.
The new program requires hospitals to make significant changes to their financial assistance policies, including: offering discounts ranging from 50 percent to 100 percent to low-income patients, capping the patients’ interest rates on hospital-held medical debt at 3 percent, proactively screening all patients for financial aid eligibility, and agreeing not to report medical debt to credit agencies.
The hospitals must make some of the changes by Jan. 1, 2025, and others over the next year. By March, they must enter into an agreement with a vendor to help facilitate debt forgiveness for low-income patients. The actual debt relief is expected to take longer.
Also in 2024, the five hospitals responsible for nearly all of North Carolina’s lawsuits filed against patients for medical debt said they would erase all of their existing judgments.
Hospitals nationwide have faced growing pressure to reform their debt collection and billing practices as the number of Americans struggling with medical debt soars.
A 2024 poll found that nearly two-thirds of North Carolinians find it somewhat or very difficult to afford health care costs, with about 1 in 5 describing it as “very difficult.”
— Michelle Crouch
Honorable mention:
Take heed, oral health providers say: No weed or gummies before your trip to the dentist.
NC HealthNews readers are often drawn to stories about marijuana and hemp laws, and that proved to be the case again this year.
Now that more states have legalized marijuana for medicinal or recreational use, the American Dental Association says more oral health care providers are seeing an increasing number of patients under the influence.
Although North Carolina has not yet joined those states, a smattering of dentists have issued guidance for patients thinking of calming their nerves before a visit with gummies or other marijuana products. Bobby White, chief executive and legal counsel for the North Carolina State Board of Dental Examiners, told NC Health News the issue is on the board’s radar but has not generated a lot of complaints.
Yet.
— Anne Blythe
The post From abortion to Hurricane Helene to medical debt, here’s what drew readers to NC Health News in 2024 appeared first on North Carolina Health News.
